Diploma
Diploma in Implant Dentistry & Prosthetic Dentistry (International) (RCSEd)
This is an international program co-organized by The Ninth People Hospital, Shanghai Jiao-tong University and The Hong Kong Institute of Implant Dentistry. This international program is also accredited by The Royal College of Surgeons of Edinburgh. This is the first of this kind of a structured program taking the participant from basic to intermediate level in Implant Dentistry and Prosthetic Dentistry. The purpose of this program is to provide adequate training including the fundamental principles and the latest developments in Implant Dentistry and Prosthetic Dentistry to clinicians who would like to perform surgical and restorative procedures relating to dental implants in their daily practice. This program aims at delivering both practice-based knowledge and skills underpinned by the relevant evidence to clinicians so that they are competent to carry out high quality practice in the field of Implant Dentistry and Prosthetic Dentistry to their patients.


Aims of the Programme:
- The programme focusing on the core knowledge and competence in the field of implant dentistry. It is intended to stress on the competency in accurate diagnosis, formulation of treatment planning and performance in implant surgery at a level of minor augmentation. More advanced procedures such as major bone grafting are not included in this programme.
- Practice Standards have been developed to ensure patient safety and protection. They should be used by dental teams and providers of training, to ensure consistency in the acquisition of knowledge and clinical skills for implant procedures, and to ensure good practice. They also serve as a reference point in the consideration of patient complaints against dentists who have allegedly practised implant dentistry without the necessary competence.
- It is essential that any patient considering dental implant treatment should receive a thorough assessment, treatment and maintenance plan, in order to give their informed consent before undergoing the procedure. The patient must receive sufficient information on the nature, risks, costs, alternatives and likely prognosis.
Eligibility:
To be eligible for the award of the Diploma, all candidates must provide evidence of having complied with all parts of the Regulations, full attendance in all classes and passing all examinations; the successful candidate will be awarded the “Diploma in Implant Dentistry (Dip Imp Dent. RCS Ed.) ” by The Royal College of Surgeons of Edinburgh, and a “Diploma in Implant and Prosthetic Dentistry ” by the School of Stomatology, the Ninth People’s Hospital of Shanghai Jiao Tong University.

Entrance Requirements:
Possession of a primary dental qualification that is acceptable to the Local Dental Council.
Having been working as a qualified dentist for at least two years, including the completion of 12 months’ full-time postgraduate experience in dentistry (general practice, hospital, community, academic or armed forces).
Course Structure:
The course structure is delivered over 5 modules which include the following:
- General Aspects
- Surgical Aspects
- Restorative Aspects
- Maintenance care
Each module is delivered over a 3 day programme using a face to face (direct contact) approach via taught structured sessions conducted over a minimum of 80 hours. Each module covers different level of knowledge and skills over the general, surgical, restorative and maintenance aspects of implant dentistry. Participants will also be expected to complete the following as part of the requirement during the 2 year period:
- Portfolio of Clinical cases: 4 clinical cases of specified indicationsusing a specified template
- Clinical observations: These will take placed in associated/accredited clinical bases. Currently there are 2 bases in Shenzhen, China, namely Shenzhen University General Hospital and Shenzhen Luohu People’s Hospital.
- Written Assignments: Based on 12 relevant topics in implant and prosthetic dentistry
- Log book of activity related to implants and associated activities: Can include attendance at teaching clinics, meetings, conferences, seminars and must incorporate a learning outcome and reflective comment
Modules 1-4 will be held in The Ninth People Hospital, Shanghai Jiao-tong University and Module 5 will be conducted in the UK.
A final examination will mark the end point of the course. The details of this examination are currently being finalized and will be announced later.
All participants who have met the following criteria during the course will be signed up to sit the final examination.
- Attendance at all taught structured sessions
- Submission of 4 completed clinical cases
- Attend the allocated clinical observation session
- Submit all written assignments within the allocated time frames
- Submission of a completed log book which will include 5 single units, 4 three units and 2 edentulous cases
- Introduction: diploma of implant dentistry
- soft tissue consideration in implant therapy
- Anatomical consideration in implant therapy
- Socket healing and socket management
- Implant design in geometry and material
- Replacement of missing tooth/teeth: treatment options and their evidence
- Modern radiographic imaging in implant treatment
- An overview of procedures and techniques of implant surgery
- Pre-therapy examination and assessment
- Medical consideration for dental implant therapy
- Overview of guided surgery
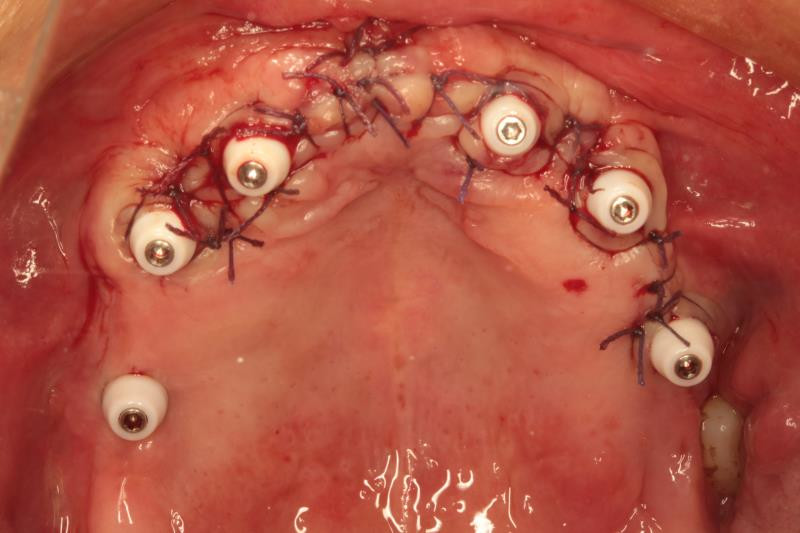
- Flap design and suture technique
- Emergency in dental clinic
- Communication, principles of consent
- Timing of implant placement and loading protocol
- SAC assessment in implant therapy
- Digital workflow in implant dentistry
- Hands-on: incision design, flap design, suture technique
- Mock examination
- Surgical concepts and principles of implant surgery(first stage and second stage)
- Anesthesia and patient monitoring
- Use of cone beam computed tomography in implant dentistry
- Evidence of immediate loading
- Role of autogenous bone
- Pre-therapy examination and assessment
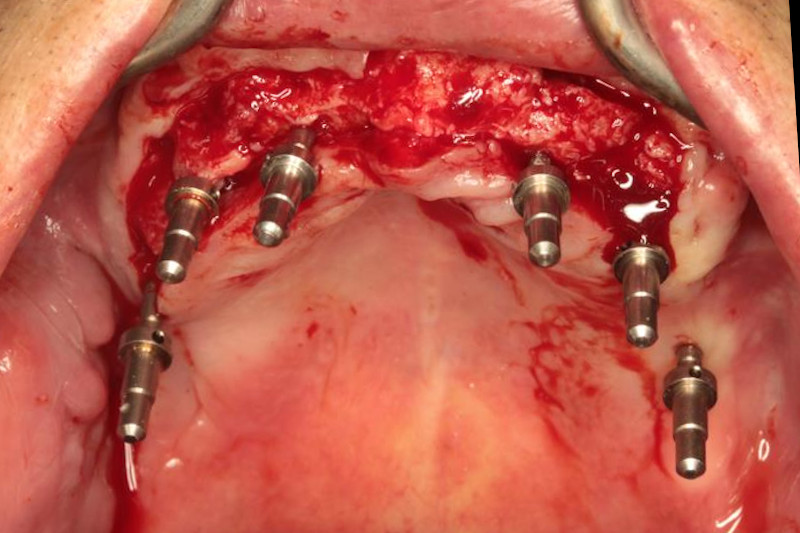
- Surgery: live demonstration
- Evidence of immediate implantation& placement
- Bone harvesting techniques
- types of augmentation material
- Principles of minor augmentation and materials
- Principle of guided bone regeneration
- Hands on: bone grafting
- Examination techniques
- Mock examination
- Lateral window approach for maxillary sinus floor elevation
- Alveolar crestal approach for maxillary sinus floor elevation
- Prosthodontic planning principles for implant placement
- Demonstration: maxillary sinus floor elevation (lateral window approach)
- Demonstration: maxillary sinus floor elevation (alveolar crestal approach)
- Superstructure design and material selection for implant prosthesis
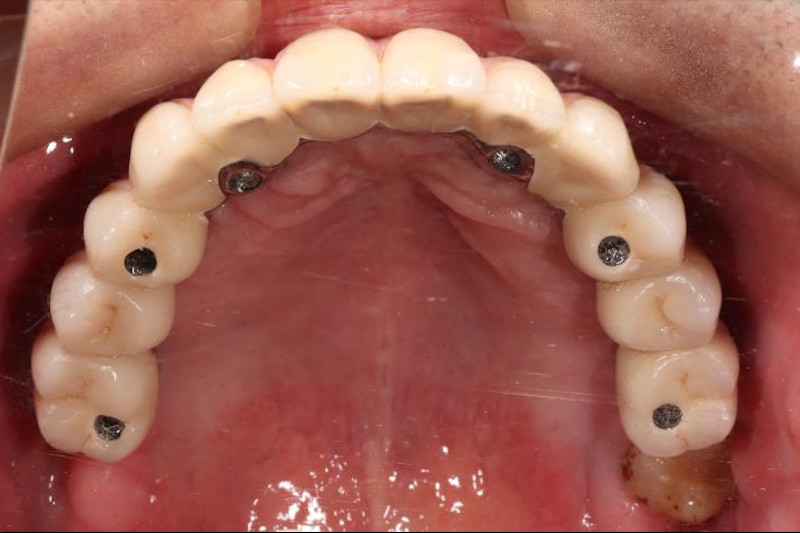
- Implant supported overdenture
- Monitoring peri-implant tissue health
- Maintenance scheme for dental implants
- Hands-on: impression taking (conventional and digital) and occlusional registration
- Hands-on: fitting of cement/screw-retained implant prosthesis
- Mock examinations (OSCE and written examination)
- Abutment selection
- Treatment plan for implant restorations: fixed vs removable, number of fixtures, materials, communication with patients)
- Transitional denture: types, procedures, implications
- Prosthetic-driven surgical planning
- Implant restorations: role of the dental laboratory
- Case study: replacement of missing anterior single tooth, missing posterior single tooth, multiple missing teeth, edentulous arch with implant-supported restorations
- Fabrication of implant-supported overdentures and transitional dentures
- How does TMD play a role in dental implant treatment?
- Marginal bone loss in dental implant and oral hygiene maintenance
- Clinical procedures of restoring implant supported fixed prostheses
- Case presentation by candidates
- Mock examination
- Lecture: peri-implantitis and implant complications – Eastman Dental Hospital (London)
- Educational tour – Edinburgh, Scotland
- Prep course – RCSEd (Scotland)
Curriculum of the International Implant Dentistry & Prosthodontics Program:
- General
- Surgical
- Restorative
- Maintenance
Basic level
- Scientific basis of Dental Implants including the concepts of osseointegration, implant systems, implant surfaces, prosthetic connections
- Treatment options for replacing failing and missing teeth including the evidence base
- Treatment planning for the implant patient I: Healthy vs periodontally compromised patient
- Treatment planning for the implant patient II: Diagnostic aides and imaging
- Treatment Planning for the implant patient III: Surgically Vs. Prosthetically driven placement
- Treatment Outcomes: Success vs Survival
- Infection control: Asepsis and Sterilization
- TMJ and Occlusion in Implant Dentistry
- TMJ MRI-measurement and assessment
- Joint-jaw-occlusion combined treatment concept
- TMJ condylar resorption and unstable occlusion
- Materials in Implant Dentistry and Prosthetic Dentistry
- Evidence based treatment planning
Intermediate level
- Complications associated with Implants including failure using an evidence based approach
- Peri-implant Tissue: In health and disease
- Surgical placement: immediate, early, delayed or standard
- Restoring implants – immediate, early or standard
- Restoring implants – Loading Protocols including criteria for immediate loading
- Digital Workflows in Implant Dentistry – from impressions to restoration
- Hard and soft tissue augmentation to enhance treatment outcomes
- Joint-jaw-occlusion combined treatment protocol
Basic level
- Anatomical considerations including site assessment relevant to dental implant
- Pain control and management for surgical intervention (eg local anesthesia; Sedation)
- Standard implant placement in the edentulous patient for denture retention
- Standard implant placement for single tooth replacement (straightforward case)
- Standard Implant placement in the partially dentate patient (straightforward case)
- Socket preservation following tooth extraction
- Clinical anatomy of TMJ
Intermediate level
- Implant placement in the aesthetic zone
- Immediate implant in non-infected sockets
- Simultaneous implant placement with guided bone regeneration (contour augmentation)
- Simultaneous implant placement with internal sinus lift procedure
- Staged implant placement following Ridge Augmentation with onlay block graft (intraoral)
- Staged implant placement following external sinus lift procedure
- Computerised planning using CADCAM techniques to provide static guides for surgery
- Computer aided dynamic navigation for implant placement
- Guided surgery and navigation
- Surgical disc repositioning
- Joint reconstruction
Single-Unit to Multi-Unit Restoration:
Basic level
- Prosthetically-driven treatment planning
- Role of the existing prosthesis
- Role of temporary prosthesis
- Impression techniques and materials
- Range of prosthetic components
- Abutment selection
- Comparison between screw-retained and cement-retained restorations
- Platform shifting: its significance and relevant evidence
- Abutment materials
- Treatment options
- Fixed and removable prosthesis
- number of implants
- materials of the prosthesis
- communication and decision making with the patient
- Fitting of a prosthesis
- Procedures involved
- Assessment and management of a mis-fitting prosthesis or framework
- Communication with the dental laboratories
- Functional training after TMJ surgery
Intermediate level
- Provisionalization: options, procedures, and significance of a provisional restoration
- Prosthetically-driven treatment planning: moving from dentures to fixed prosthesis
- Conversion of a removable prosthesis into a provisional implant-retained or implant-supported prosthesis
- Role of digital techniques in
- Treatment planning
- Communication with patients
- Surgical planning
- Fabrication of prosthesis
- Prosthetic complications: prevention and management and their evidence
- Prothodontics following TMJ surgery
- Mandibular repositioning after disc reposition
- Treatment planning with joint reconstruction
- Occlusion reconstruction in TMJ tumor, anakylosis, and faical trauma
Occlusion in implant dentistry:
Basic level
- Occlusion in natural teeth
- Ideal occlusion
- Occlusal schemes
- Mutually protected occlusion
- Occlusion in implant restorations
- Occlusal guidelines for different situations: Single implant vs multi-unit vs full mouth rehabilitation
- Implant-protected-occlusion
- Occlusal stability and TMJ stability
Intermediate level
- Difference between teeth and implants in occlusion
- Considerations before implant restorations
- Assessment of TMJ before implant restorations
- Orthodontics following TMJ surgery
- Stable occlusion and the use of soft splint
- Comparison betweenReposition splint, herbst and twin-block
- Anterior repositioning appliancesand bone regeneration
- Orthognathic interventions
- Complications of compromised design in occlusion and its prevention
- Jaw registration: procedures and techniques
- Temporomandibular joints – bruxists and myofascial pain
- Maintenance around implants including oral hygiene instruction
- Marginal Bone Changes: Theories and their related evidence
- Peri-implant disease – Prevention, diagnosis, management and their evidence
- Prosthetic failures
- Complications: short and long term
- Communciation with the patient

Training and Examination:
Training and Examination Centre in Implant and Prosthetic Dentistry of
the Royal College of Surgeons (Edinburgh) and the Ninth People’s Hospital of Shanghai Jiaotong University
Head: Prof. Wu Yi Qun
Clinical Bases:
Shenzhen University General Hospital, Shenzhen, Guangdong
Head: Prof. Deng Yong Qiang
Shenzhen Luohu People’s Hospital, Shenzhen, Guangdong
Head: Prof. Muhetaer Huojia
Application:
Applicants will be required to provide a current curriculum vitae and covering letter in support of their application. The prerequisite for acceptance on the program is a registrable qualification/license to practice dentistry.